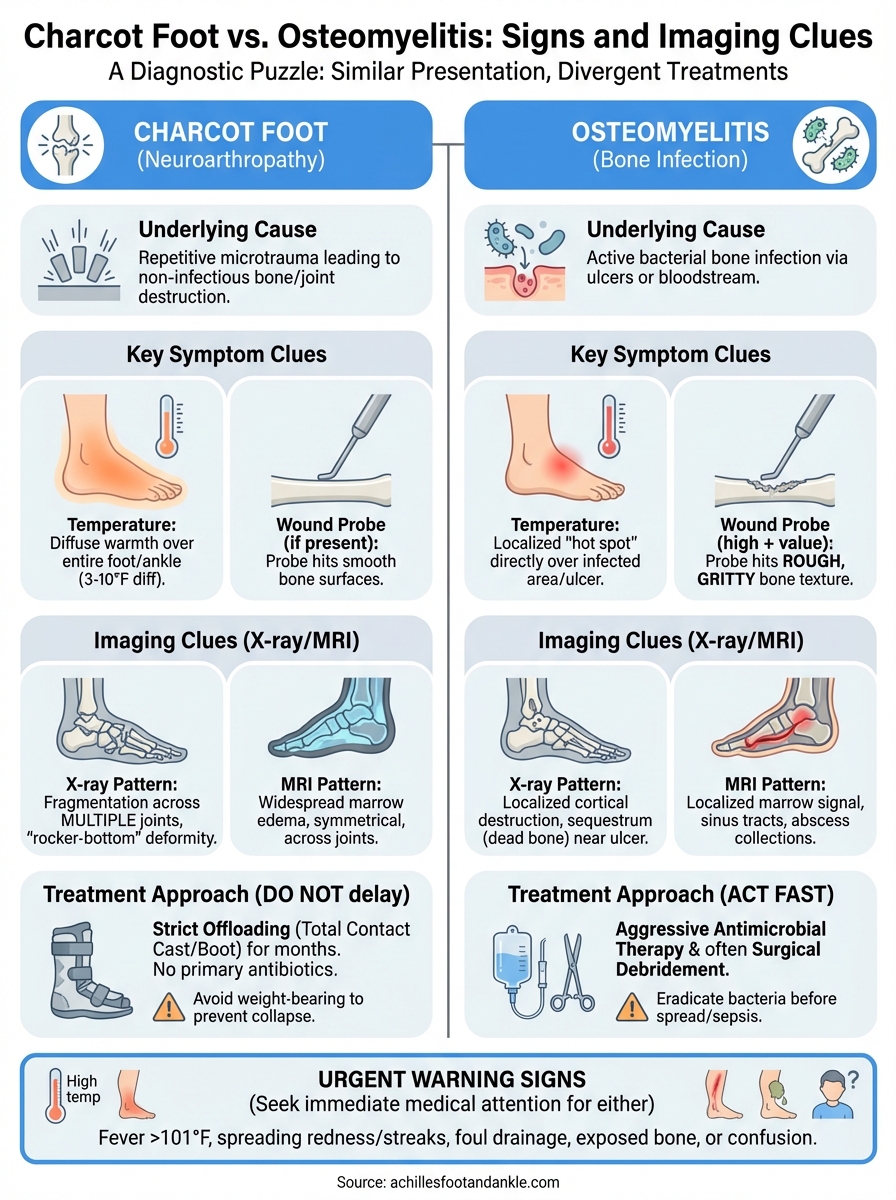
A swollen, red, warm foot in a patient with diabetes or peripheral neuropathy presents a diagnostic puzzle that even experienced clinicians find challenging. The distinction between Charcot foot vs osteomyelitis matters because these two conditions require completely different treatment approaches, yet they share remarkably similar clinical presentations. Missing the correct diagnosis can lead to unnecessary amputations, prolonged infections, or progressive joint destruction.
Both conditions commonly affect patients with reduced sensation in their feet, and both can cause significant swelling, erythema, and structural changes visible on imaging. However, Charcot neuroarthropathy involves bone and joint destruction from repetitive microtrauma, while osteomyelitis represents active bone infection that spreads from overlying ulcers or through the bloodstream. The overlap in symptoms and imaging findings makes accurate differentiation essential for proper treatment planning.
At Achilles Foot and Ankle Center, our team regularly evaluates complex foot presentations requiring advanced diagnostic imaging and clinical expertise. This guide breaks down the key signs, imaging characteristics, and diagnostic criteria that help distinguish between these two serious conditions, giving you the information you need to understand what’s happening and seek appropriate specialized care when symptoms arise.
Why the difference matters
The consequences of misdiagnosing Charcot foot vs osteomyelitis extend far beyond simple treatment adjustments. Getting the diagnosis wrong can mean putting a patient on prolonged antibiotics they don’t need while their bone structure collapses uncontrolled, or failing to treat a serious infection that spreads deeper into tissue and bone. Each condition follows a distinct disease process that demands specific interventions, and mixing them up leads to preventable complications.
Treatment paths diverge completely
Osteomyelitis requires aggressive antimicrobial therapy, often lasting six weeks or longer with intravenous antibiotics initially, followed by oral medications tailored to culture results from bone biopsies. You might need surgical debridement to remove infected bone tissue, and in severe cases, the infection can necessitate partial foot amputation to prevent sepsis and save the limb. The entire treatment strategy centers on eradicating bacteria from bone tissue before the infection destroys more tissue or enters your bloodstream.
Charcot foot demands the opposite approach: complete offloading and immobilization to allow the inflammatory phase to resolve and the bone to heal in a functional position. Your foot care team will typically use a total contact cast or specialized boot to eliminate all weight-bearing forces while the acute phase settles over three to six months. Antibiotics play no role unless you develop a secondary infection, and surgery becomes necessary only if conservative management fails or if structural deformities require reconstruction after the acute inflammation subsides.
The treatment for one condition can actively harm a patient with the other, making accurate diagnosis critical before starting any intervention.
Timing affects outcomes dramatically
Osteomyelitis that goes untreated for even a few weeks allows bacteria to establish deeper biofilms within bone tissue, making eradication progressively harder and increasing the risk of treatment failure. The infection can spread to adjacent joints, tendons, and soft tissue structures, expanding the zone of tissue that requires surgical removal. You face mounting risks of systemic infection and sepsis if the bacteria enter your bloodstream, which can rapidly become life-threatening without immediate intervention.
Delayed recognition of acute Charcot foot means continued weight-bearing on unstable bone fragments, which drives progressive joint destruction and permanent deformity. The fragmented bones collapse into abnormal positions that create pressure points, virtually guaranteeing future ulceration even after the acute phase resolves. Starting proper offloading within the first weeks of symptoms can preserve your foot architecture, while waiting months often means you’ll need complex reconstructive surgery to achieve a plantigrade, stable foot capable of bearing weight safely.
Cost and recovery trajectories differ substantially
Treating osteomyelitis typically involves hospitalization for intravenous antibiotics, multiple surgeries for debridement, extended wound care visits, and potential home health services for continued IV therapy. The total cost regularly exceeds tens of thousands of dollars, and recovery timelines stretch across months with ongoing risks of recurrence. You may need serial imaging studies to monitor bone healing and confirm infection resolution, adding to both time and financial burden.
Charcot foot management relies primarily on outpatient casting and regular monitoring, avoiding hospitalization in most cases and keeping costs substantially lower initially. However, if you develop severe deformity from delayed diagnosis, the reconstructive surgery and recovery period can rival or exceed osteomyelitis treatment costs. Your ability to return to work and normal activities depends heavily on catching the condition early and maintaining strict offloading protocols throughout the acute phase, typically requiring four to six months of modified activity before you can safely resume full weight-bearing.
Key symptom and exam clues
Your clinician faces a significant challenge when examining a swollen foot, because Charcot foot vs osteomyelitis presentations overlap substantially at first glance. Both conditions create redness, warmth, and swelling that can look identical in photos or casual observation. However, systematic physical examination reveals subtle but consistent differences in temperature patterns, vascular status, wound characteristics, and structural findings that guide accurate diagnosis before imaging studies even begin. Understanding these clinical clues helps you recognize which condition might be affecting your foot and why your doctor performs specific examination maneuvers.
Temperature differences you can detect
Temperature asymmetry provides one of the most reliable clinical indicators distinguishing these conditions. Acute Charcot foot typically produces a 3 to 10 degree Fahrenheit temperature increase compared to your unaffected foot, measurable with an infrared thermometer at multiple points across the dorsum and plantar surfaces. The warmth spreads diffusely across the entire foot and ankle region, reflecting the widespread inflammatory response throughout the bone and joint structures without localized infection.

Osteomyelitis generates heat concentrated around the infected bone and overlying ulcer, with normal or near-normal temperatures elsewhere on your foot. You can often identify the specific infected area by comparing temperatures at different sites, finding a hot spot that corresponds to bone involvement rather than generalized warmth. The infected tissue feels warmer than adjacent healthy tissue, creating a localized thermal gradient your clinician can map during examination.
Temperature monitoring over several days helps track disease progression, with persistent elevation suggesting active infection while gradual cooling indicates successful treatment response.
What probing the wound reveals
The probe-to-bone test delivers critical diagnostic information when you have an open ulcer on your foot. Your doctor inserts a sterile metal probe through the wound base, and direct contact with rough, gritty bone texture strongly suggests osteomyelitis involvement with positive predictive values exceeding 90% in published studies. The probe passes easily through infected soft tissue until it encounters compromised bone, which feels distinctly different from normal granulation tissue.
Charcot foot patients without secondary infection show no ulceration initially, or if wounds develop from pressure points, probing encounters only soft tissue and smooth bone surfaces without the roughened texture characteristic of infected bone. Your wound care specialist performs this test gently to avoid creating false passages, interpreting results alongside other clinical findings rather than relying on probe-to-bone testing alone. The presence of exposed bone fragments in Charcot feet indicates advanced destruction rather than infection, requiring different treatment protocols.
Imaging clues on X-ray, MRI, and nuclear scans
Radiographic imaging provides the definitive evidence your clinician needs to distinguish Charcot foot vs osteomyelitis, revealing bone and soft tissue changes invisible during physical examination. Standard X-rays serve as your first-line imaging tool, showing skeletal abnormalities with excellent spatial resolution at low cost. However, plain radiographs miss early disease changes and soft tissue infections, prompting your foot specialist to order advanced imaging studies when X-ray findings remain ambiguous or clinical suspicion stays high despite negative initial films.
X-ray findings that point to each condition
Plain radiographs in acute Charcot foot demonstrate fragmentation patterns, subluxation, and dislocation across multiple joints, typically affecting the midfoot in characteristic distributions. You’ll see bone debris, fracture lines through multiple metatarsals or tarsal bones, and joint spaces widening as ligaments fail. The destruction follows predictable anatomic locations like the Lisfranc joint or tarsometatarsal articulations, creating the classic "rocker-bottom" deformity in advanced cases with progressive collapse of the arch structure.
Osteomyelitis creates more localized changes concentrated around one or two bones adjacent to your ulcer site. The infected bone shows cortical destruction, periosteal reaction, and sequestrum formation (dead bone fragments separated from living tissue). Your radiologist looks for focal lucency, irregular bone margins, and soft tissue gas in severe infections rather than the diffuse fragmentation spanning multiple joints seen in Charcot changes.
MRI patterns that separate the two
Magnetic resonance imaging reveals bone marrow edema in both conditions, but the distribution patterns differ substantially. Charcot foot produces widespread marrow signal changes affecting multiple bones symmetrically with subchondral cysts and extensive joint effusions. The edema spreads beyond any single anatomic compartment, involving bones on both sides of affected joints without the focal abscess collections characteristic of infection.
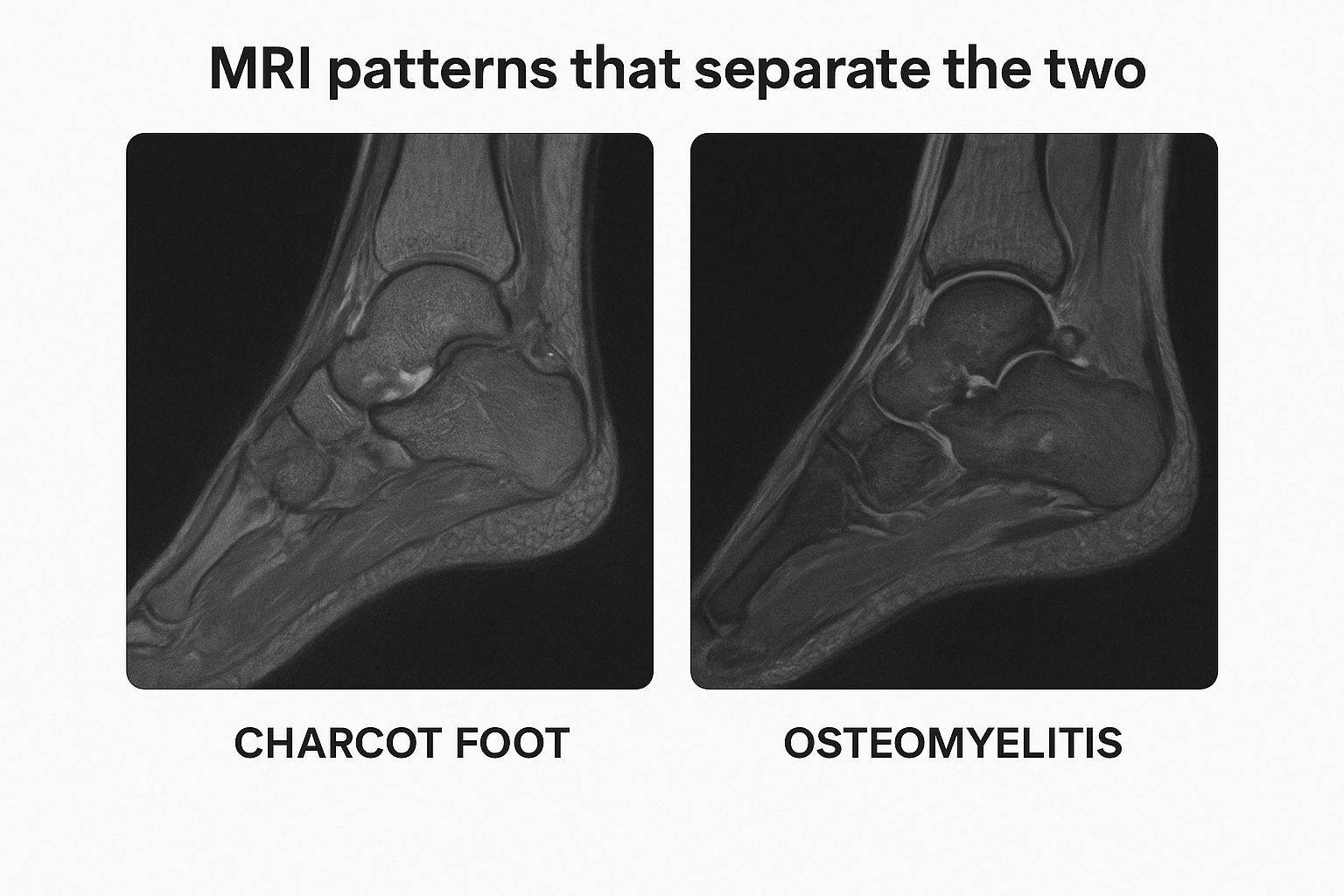
Osteomyelitis demonstrates localized bone marrow replacement with abnormal signal, sinus tracts connecting ulcers to bone, and rim-enhancing fluid collections suggesting abscess formation. Your radiologist identifies contiguous spread from the wound site into adjacent bone rather than the skip lesions and diffuse involvement typical of Charcot neuroarthropathy. Soft tissue enhancement patterns help distinguish sterile inflammation from infected tissue requiring surgical drainage.
MRI sensitivity exceeds 90% for detecting bone infections, but specificity drops when inflammation from Charcot mimics infectious changes, requiring correlation with clinical findings and laboratory markers.
Nuclear medicine when standard imaging leaves doubt
White blood cell scans labeled with indium-111 or technetium-99m accumulate at sites of active infection, helping confirm osteomyelitis when MRI findings remain equivocal. These nuclear studies show focal uptake at infected bone sites while Charcot foot produces more diffuse uptake throughout the inflamed region. Combined bone and white cell scanning improves diagnostic accuracy by highlighting metabolic activity patterns that distinguish infection from sterile inflammation, though you’ll wait 24 to 48 hours for delayed imaging that captures the full pattern.
A practical diagnostic approach step by step
Your clinician follows a systematic evaluation process when confronting the Charcot foot vs osteomyelitis diagnostic challenge, integrating clinical findings with laboratory data and imaging studies in a logical sequence. This structured approach minimizes diagnostic errors while avoiding unnecessary testing costs and radiation exposure. Understanding each step helps you recognize why your doctor orders specific tests and how the pieces fit together to reach an accurate diagnosis.
Start with thorough history and physical examination
Your evaluation begins with documenting risk factors specific to each condition, including diabetes duration, previous foot ulcers, recent trauma, and the timeline of symptom development. Charcot foot typically develops over days to weeks with progressive swelling but minimal pain due to neuropathy, while osteomyelitis usually follows weeks to months after an ulcer appears with gradual worsening despite topical treatments. Your doctor examines both feet carefully, comparing temperatures, checking for skin breaks, and assessing your protective sensation with monofilament testing to establish your baseline neuropathy level.
The physical examination focuses on identifying wound characteristics if ulceration exists, including depth, drainage quality, and whether probing reaches bone. Your specialist documents the exact location and extent of erythema and swelling, measures foot temperatures with an infrared thermometer, and tests your vascular status through palpable pulses or ankle-brachial index measurements. These baseline findings guide subsequent testing decisions and provide reference points for tracking your response to treatment over time.
Order targeted laboratory studies next
Blood work provides supporting evidence rather than definitive diagnosis in most cases. Your doctor checks inflammatory markers including erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), which typically elevate above 70 mm/hr and 10 mg/L respectively in osteomyelitis but may also rise in acute Charcot foot. White blood cell counts remain normal in both conditions unless you develop systemic infection requiring urgent intervention. Hemoglobin A1c testing reveals your glucose control status, which affects both disease risk and healing capacity regardless of the final diagnosis.
Laboratory values alone cannot distinguish between these conditions, requiring integration with clinical and imaging findings for accurate diagnosis.
Follow a strategic imaging sequence
Plain radiographs of both feet serve as your initial imaging study, allowing direct comparison between affected and unaffected sides. Your radiologist reviews the films for bone destruction patterns, joint involvement distribution, and soft tissue changes that suggest one diagnosis over another. If X-rays show clear Charcot changes with fragmentation across multiple joints and no wound connection, you may proceed directly to offloading treatment without additional imaging costs.
When radiographs remain inconclusive or show changes consistent with either condition, MRI becomes your next step. The scan reveals bone marrow edema distribution, abscess collections, and sinus tract formation that X-rays miss entirely. Your foot specialist orders nuclear medicine studies only when MRI findings stay equivocal or when you have contraindications like pacemakers preventing magnetic resonance imaging.
Treatment implications and when to seek urgent care
Understanding the difference between Charcot foot vs osteomyelitis directly determines whether you need antibiotics, immobilization, or urgent surgical intervention. Your treatment pathway diverges completely based on accurate diagnosis, and starting the wrong therapy can worsen your condition significantly. Recognizing when your symptoms require immediate medical attention versus scheduled specialist visits helps you avoid preventable complications while ensuring timely access to the care you need.
Treatment protocols differ fundamentally
Osteomyelitis requires antimicrobial therapy tailored to culture results, typically starting with broad-spectrum intravenous antibiotics until bone biopsy identifies the specific bacteria. Your infectious disease team adjusts medications based on sensitivity testing, and you may need six to twelve weeks of treatment depending on how deeply the infection penetrated your bone. Surgical debridement removes dead tissue and infected bone fragments, creating clean margins that allow antibiotics to work effectively while reducing bacterial load that medications alone cannot eliminate.
Charcot foot demands strict offloading protocols using total contact casts or specialized walking boots that eliminate all pressure on your affected foot. Your podiatrist changes casts every one to two weeks initially, monitoring for skin breakdown and adjusting as swelling decreases. You must avoid weight-bearing completely for three to six months while the inflammatory phase resolves, and premature return to activity restarts the destructive cycle. Surgical reconstruction becomes necessary only if conservative management fails or severe deformity develops, requiring osteotomy and internal fixation to restore your foot architecture.
Mixing up these conditions means giving antibiotics to someone who needs immobilization, or immobilizing someone who needs urgent infection control, both leading to serious harm.
Emergency warning signs requiring immediate evaluation
You need urgent medical attention within hours if you develop fever above 101°F, spreading redness that advances beyond your foot, red streaking up your leg, confusion, or rapid heartbeat. These symptoms suggest systemic infection that can quickly progress to sepsis, requiring hospitalization and intravenous antibiotics to prevent life-threatening complications. Your emergency department will obtain blood cultures, start broad-spectrum antibiotics, and arrange imaging to assess infection extent before transferring you to specialized care.
Sudden worsening of swelling, new-onset severe pain despite your neuropathy, foul-smelling drainage, or exposed bone through your wound also warrant same-day evaluation even without fever. These findings indicate advancing infection or acute Charcot collapse requiring immediate intervention to prevent permanent damage. Contact your podiatrist or visit an urgent care facility capable of arranging specialist consultation rather than waiting for regular office hours when these warning signs appear.
Next steps for your foot
Distinguishing between Charcot foot vs osteomyelitis requires specialized expertise and advanced diagnostic tools that go beyond standard primary care examinations. Waiting for your symptoms to resolve on their own means risking permanent foot deformity or spreading infection, both of which can lead to amputation or lifelong disability. Your foot health depends on getting accurate diagnosis and starting appropriate treatment as quickly as possible after symptoms appear.
At Achilles Foot and Ankle Center, our experienced podiatrists use comprehensive physical examinations, advanced imaging interpretation, and evidence-based protocols to distinguish between these challenging conditions. We offer same-day appointments for urgent foot concerns, giving you rapid access to specialized care when every day counts toward preventing complications. Contact our team today if you’re experiencing unexplained foot swelling, warmth, or redness, especially if you have diabetes or peripheral neuropathy that puts you at higher risk for these serious conditions.