That persistent numbness or burning sensation across the top of your foot isn’t something you should ignore. When these symptoms appear, especially during walking or exercise, you may be dealing with superficial peroneal nerve entrapment ankle, a condition where the nerve becomes compressed as it travels through the lower leg and ankle. Left untreated, this compression can lead to chronic pain and sensory changes that affect your daily activities.
Understanding what’s causing your symptoms is the first step toward relief. At Achilles Foot and Ankle Center, our podiatrists regularly diagnose and treat nerve entrapment conditions using advanced diagnostic technology and individualized treatment plans tailored to each patient’s needs.
This article covers everything you need to know about superficial peroneal nerve entrapment, from recognizing the early warning signs to exploring conservative care and surgical options that can restore comfort and function to your foot and ankle.
Why superficial peroneal nerve entrapment happens
The superficial peroneal nerve travels from your lower leg down toward your ankle, passing through several tight spaces where compression can occur. This nerve controls sensation across the top of your foot and helps with certain ankle movements, making it vulnerable to pressure from surrounding structures.
Anatomical structures that trap the nerve
Your superficial peroneal nerve typically exits the deep compartment of your leg through an opening in the fascial tissue located approximately 10 to 13 centimeters above your lateral malleolus (the bump on the outside of your ankle). At this exit point, the nerve becomes more superficial and exposed to external pressure. When the fascia narrows or thickens, it creates a bottleneck that squeezes the nerve against nearby bones and muscles.
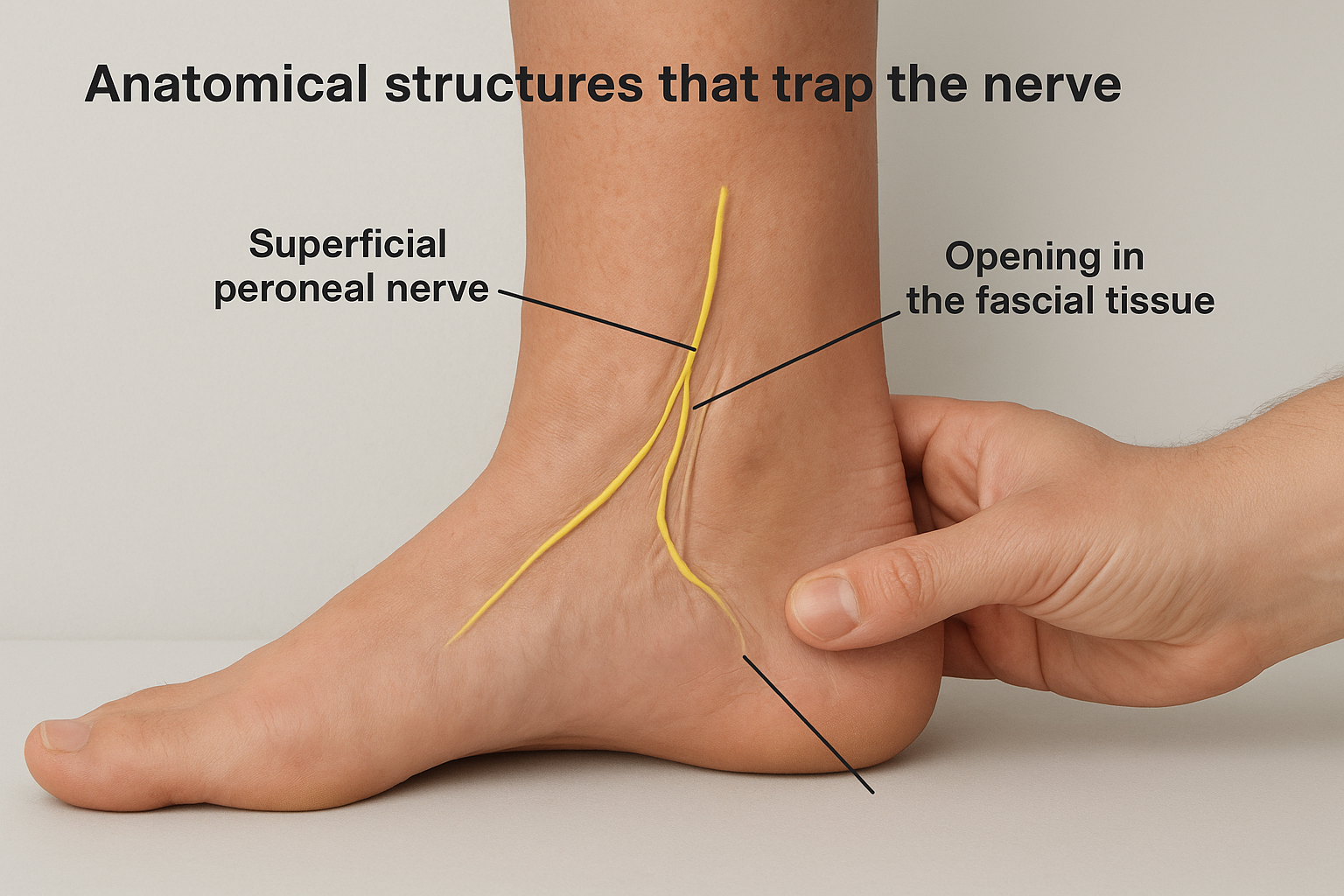
Variations in your anatomy can also contribute to entrapment. Some people have tighter fascial openings naturally, while others develop scar tissue from previous injuries that restricts the space available for the nerve. The nerve may also take an unusual anatomical path in certain individuals, making it more susceptible to compression during normal activities.
Repetitive movements and direct trauma
Athletes who participate in activities requiring repeated ankle inversion (rolling the ankle inward) face higher risk of developing superficial peroneal nerve entrapment ankle symptoms. Running, jumping, and cutting movements force the nerve to stretch and compress repeatedly, leading to inflammation and eventual entrapment. Soccer players, dancers, and runners commonly experience these issues.
Direct trauma to the outer leg or ankle can also damage the nerve or surrounding tissues. An ankle sprain creates swelling that puts pressure on the nerve, while a direct blow to the area can cause immediate compression. Previous surgeries near the nerve pathway may result in scar tissue formation that gradually restricts nerve movement.
Athletes and active individuals who ignore early symptoms of nerve irritation often develop chronic entrapment that requires more intensive treatment.
Medical conditions that increase compression risk
Certain systemic conditions make you more vulnerable to nerve problems throughout your body. Diabetes affects nerve health by reducing blood flow and causing metabolic changes that damage nerve tissue. People with diabetes may not notice early entrapment symptoms because they already experience baseline numbness or altered sensation.
Compartment syndrome, whether acute or chronic, raises pressure within the leg’s muscular compartments and can trap the superficial peroneal nerve at its exit point. Previous ankle fractures or dislocations alter the normal anatomy and create new pressure points that weren’t present before injury. Occupation-related factors also play a role when your job requires prolonged standing or repetitive leg movements that strain the nerve over time.
Symptoms you can feel in the ankle and foot
Superficial peroneal nerve entrapment ankle symptoms typically develop gradually and affect the top and outer portions of your foot. You might notice tingling or burning sensations that radiate from your outer lower leg down to your toes, particularly after walking or standing for extended periods. These feelings often worsen during activities that stretch the nerve.
Sensory changes across the foot’s surface
Your skin may feel numb or hypersensitive along the top of your foot, especially between your toes and across the area where your shoelaces rest. This altered sensation can make it difficult to gauge pressure when walking, and you might find yourself stumbling or misjudging steps because your brain isn’t receiving accurate feedback from the affected area. Some patients describe a "pins and needles" feeling that persists even at rest, while others experience sharp, shooting pains that travel along the nerve pathway.
Touching the skin over the nerve may trigger immediate discomfort or electric-like sensations that radiate outward from the compression site. You could also notice that cold temperatures intensify your symptoms, making winter months particularly challenging.
Pain patterns that affect your activities
The discomfort from superficial peroneal nerve entrapment ankle often intensifies during specific movements. Pointing your foot downward or rolling your ankle inward can reproduce the pain because these positions stretch the already compressed nerve. Running, jumping, or wearing tight boots that press against the outer leg may trigger sharp, stabbing sensations that force you to stop your activity.
Activities requiring repetitive ankle motion create the most consistent symptoms because they repeatedly stress the trapped nerve.
Nighttime symptoms can also develop as swelling accumulates throughout the day and increases pressure on the nerve while you rest.
How to tell it apart from similar problems
Several conditions create pain and numbness in similar areas as superficial peroneal nerve entrapment ankle, making accurate identification crucial for proper treatment. You need to understand the distinct characteristics of nerve entrapment versus other foot and ankle problems to avoid pursuing ineffective treatments or delaying your recovery.
Compartment syndrome vs nerve entrapment
Compartment syndrome produces deep, aching pain throughout your entire lower leg that intensifies during exercise and improves with rest. Unlike nerve entrapment, this condition creates pressure within the muscle compartments rather than directly on the nerve itself. You’ll experience tightness and swelling that affects the whole leg, while superficial peroneal nerve entrapment ankle symptoms remain more localized to the nerve pathway along the outer leg and top of your foot.
The timing of symptoms also differs. Compartment syndrome pain typically builds during activity and requires you to stop completely, whereas nerve entrapment may allow you to continue moving despite discomfort. Your symptoms from compartment syndrome resolve quickly after stopping activity, while nerve irritation often persists for hours.
Distinguishing between widespread muscle pain and specific nerve pathway symptoms helps your podiatrist determine which diagnostic tests you need.
Stress fractures and tendon inflammation
Stress fractures in your foot or ankle create sharp, localized pain when you press on the bone, which differs from the radiating, electric sensations of nerve compression. Your pain from a fracture worsens with weight-bearing and improves dramatically when you rest, following a predictable pattern that nerve problems don’t share.
Tendon inflammation, particularly of the peroneal tendons, mimics some nerve symptoms but responds differently to movement. Tendonitis pain increases with specific ankle motions like pointing your foot or rolling it outward, while nerve entrapment creates symptoms during a broader range of movements. You’ll also notice visible swelling along the tendon with tendonitis, whereas nerve problems rarely cause obvious external changes.
How a podiatrist diagnoses it
Your podiatrist starts by gathering a detailed history of your symptoms, including when they began, what activities trigger discomfort, and whether any injuries preceded the pain. This conversation helps identify patterns that point toward nerve compression rather than other foot and ankle problems. The doctor will ask about your occupation, athletic activities, and any previous surgeries or trauma to your leg and ankle.
Physical examination findings
During the physical exam, your podiatrist palpates the superficial peroneal nerve pathway along your outer lower leg, searching for tenderness or a Tinel’s sign (a tingling sensation when the nerve is tapped). You may feel sharp, electric sensations radiating toward your foot when pressure is applied to the entrapment site, confirming nerve involvement. The doctor also tests your sensory perception on the top of your foot by touching various areas with light pressure or a specialized tool to map out numbness or hypersensitivity.

Specific provocative tests help confirm superficial peroneal nerve entrapment ankle. Your podiatrist may ask you to point your foot downward and inward, positions that stretch the nerve and reproduce your symptoms. Comparing strength and sensation between your affected foot and your healthy foot reveals asymmetries that indicate nerve dysfunction.
A positive Tinel’s sign at the fascial exit point, combined with sensory changes in the nerve’s distribution, strongly suggests entrapment.
Advanced diagnostic testing
When physical examination findings suggest nerve compression, your podiatrist may order electrodiagnostic studies like nerve conduction velocity tests and electromyography (EMG) to measure how well electrical signals travel through the nerve. These tests reveal slowed conduction or abnormal signals at the entrapment site, confirming the diagnosis and ruling out nerve problems originating from your spine or elsewhere.
Imaging studies help identify structural causes of compression. Ultrasound visualizes the nerve directly and shows thickening or swelling at the entrapment point, while MRI detects masses, scar tissue, or fascial abnormalities that compress the nerve. Your doctor may also use diagnostic injections of local anesthetic near the nerve to temporarily relieve symptoms, confirming both the location and source of your pain.
Treatment and recovery options
Your treatment plan for superficial peroneal nerve entrapment ankle depends on the severity of your symptoms and how long you’ve experienced them. Most patients respond well to conservative treatments that reduce nerve compression and inflammation, though some cases require surgical intervention when the nerve remains trapped despite non-invasive approaches.
Conservative treatments that reduce compression
Your podiatrist typically starts with rest and activity modification to reduce stress on the compressed nerve. You’ll need to avoid activities that reproduce your symptoms, particularly those involving repetitive ankle inversion or prolonged standing. Wearing loose-fitting footwear eliminates external pressure on the nerve pathway along your outer leg.
Physical therapy plays a central role in recovery by improving ankle mobility and reducing fascial tightness around the nerve exit point. Your therapist teaches you specific stretches that create space for the nerve and strengthening exercises that stabilize your ankle joint. Anti-inflammatory medications help control swelling that contributes to compression, while corticosteroid injections near the entrapment site provide targeted relief for persistent inflammation.
Conservative treatments resolve symptoms in approximately 60 to 80 percent of patients when started early and followed consistently.
Custom orthotics may help if your foot mechanics contribute to nerve stress by controlling excessive motion during walking and running.
Surgical intervention for persistent cases
Surgery becomes necessary when conservative treatments fail after several months or when you experience progressive numbness and weakness that indicates ongoing nerve damage. Your podiatrist performs a nerve decompression procedure that releases the tight fascia compressing the superficial peroneal nerve, creating more space for it to move freely.
Recovery from surgical release typically requires four to six weeks before you resume normal activities, with full healing occurring over three to six months. Your surgeon may remove any masses or scar tissue discovered during the procedure that contributes to compression. Post-surgical physical therapy helps restore strength and range of motion while preventing adhesions from forming around the newly released nerve.
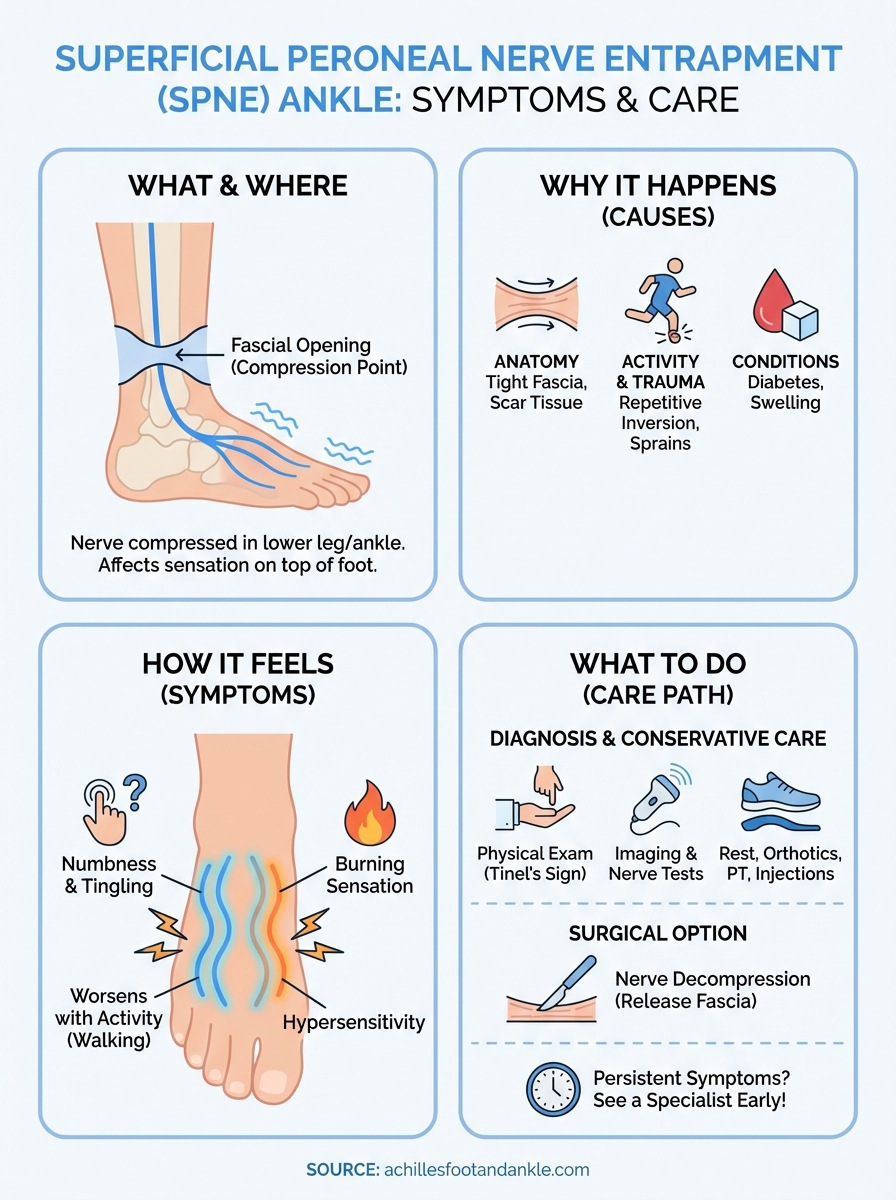
When to see a foot and ankle specialist
You should schedule an appointment when numbness, tingling, or burning sensations persist for more than a few days or worsen with activity. Early intervention prevents permanent nerve damage and shortens your recovery time. Contact a podiatrist immediately if you develop weakness in your foot or notice that your symptoms interfere with walking, running, or daily tasks.
Ignoring superficial peroneal nerve entrapment ankle symptoms allows the condition to progress, making treatment more complex and potentially requiring surgical intervention. Our team at Achilles Foot and Ankle Center uses advanced diagnostic technology to identify nerve compression and creates personalized treatment plans that address your specific needs. We offer same-day appointments when urgent symptoms develop, ensuring you receive prompt care without unnecessary delays.
Schedule your appointment today to stop nerve pain from limiting your mobility and quality of life.