Charcot foot can destroy the bones and joints of your foot within weeks, yet in its early stages, it often looks like nothing more than a swollen ankle. Understanding how Charcot foot is diagnosed makes the difference between catching this condition early and facing permanent deformity or amputation. For patients with diabetes or peripheral neuropathy, recognizing the warning signs is critical.
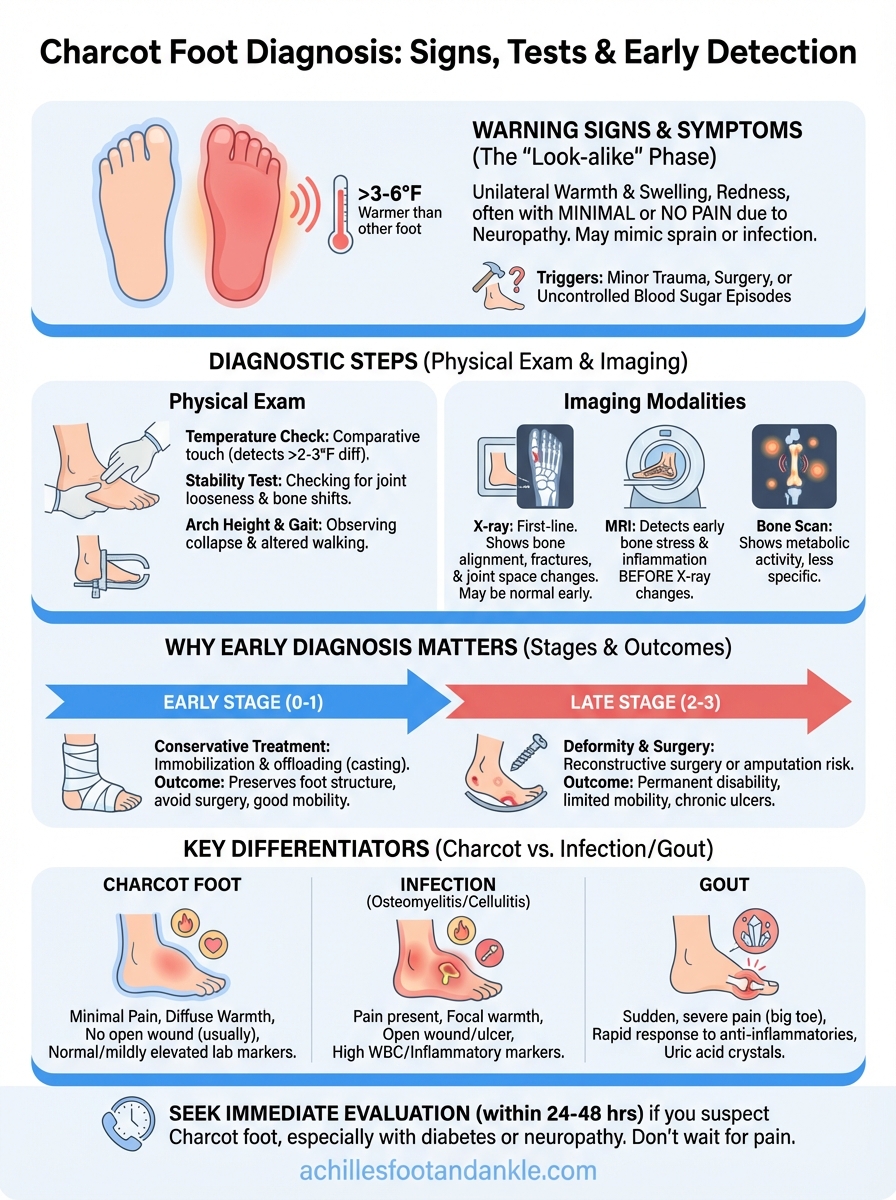
The challenge? Charcot foot mimics other common conditions. Redness, warmth, and swelling can easily be mistaken for an infection, gout, or a simple sprain. Without the right diagnostic approach, combining physical examination findings with targeted imaging, this progressive condition can advance undetected. By the time structural collapse becomes obvious on an X-ray, significant damage has already occurred.
This guide walks you through exactly what happens during a Charcot foot evaluation: the specific tests your doctor will order, what imaging reveals at each stage, and the clinical signs that separate Charcot from look-alike conditions. At Achilles Foot and Ankle Center, our specialists diagnose and treat Charcot foot across our Central Virginia locations, using advanced imaging technology and decades of combined experience in diabetic foot care to catch this condition when intervention matters most.
Why early diagnosis of Charcot foot matters
Your bones can start fracturing and your foot architecture can begin collapsing within weeks of the first symptoms appearing. The acute phase of Charcot foot progresses rapidly, and the damage accumulates silently because neuropathy masks the pain that would normally stop you from walking on a fractured foot. Every day you walk on an undiagnosed Charcot foot, you drive bone fragments deeper into surrounding tissue and accelerate joint destruction.
The difference between catching Charcot foot in stage 0 or stage 1 versus stage 2 or 3 determines whether you’ll need conservative treatment with immobilization or face reconstructive surgery and possible amputation. Understanding how Charcot foot is diagnosed early gives you the knowledge to recognize symptoms before irreversible damage occurs. Most patients who develop severe deformity had weeks or months of warning signs that were either dismissed as minor swelling or misdiagnosed as infection.
The window for non-surgical treatment closes quickly
Stage 0 and early stage 1 Charcot foot respond well to total contact casting and protected weight-bearing, treatments that cost a fraction of surgery and preserve your foot’s structure. Once you progress to stage 2, when bone fragments have shifted and joints have dislocated, you face a choice between custom bracing for life or surgical reconstruction. The inflammatory cascade that dissolves bone and weakens ligaments peaks in the first 3 to 6 months, making this your critical intervention window.
Catching Charcot foot before visible deformity develops means your doctor can stabilize the foot with 12 to 18 weeks of casting followed by gradual return to protected walking. Your foot maintains its normal shape, you avoid surgery, and you keep your ability to wear regular shoes with custom inserts. Miss this window, and you’re looking at months of recovery from surgery, metal hardware permanently implanted in your foot, and limited mobility even after healing.
Early diagnosis transforms Charcot foot from a potentially limb-threatening condition into a manageable chronic issue that preserves your quality of life.
How delayed diagnosis leads to permanent disability
Stage 3 Charcot foot creates a rocker-bottom deformity where the arch collapses completely and the midfoot bulges downward. This architectural collapse concentrates all your body weight on bones and soft tissue that were never designed to bear direct pressure. You develop chronic ulcers at pressure points that resist healing because compromised blood flow and repeated trauma prevent wound closure.

The combination of deformity and ulceration creates a pathway for deep bone infection, which accounts for 60% of diabetes-related amputations in patients with Charcot foot. Your options narrow to either complex reconstructive surgery with external fixation devices or amputation, both of which carry significant risks in patients with diabetes and neuropathy. Reconstructive surgery for advanced Charcot foot requires 6 to 12 months of recovery and still may not prevent future ulceration.
The financial and personal toll of missed diagnosis
Treatment costs escalate dramatically with each stage of progression. Total contact casting for early Charcot foot costs several thousand dollars over three to four months, while surgical reconstruction runs $50,000 to $100,000 including hospital stays, hardware, and extended recovery. Your ability to work disappears during months of non-weight-bearing recovery, and you face potential complications that require additional surgeries.
Beyond financial impact, late-stage Charcot foot steals your independence. You need help with basic activities, you can’t drive during extended periods of immobilization, and you lose the spontaneous mobility most people take for granted. Patients who catch Charcot foot early return to modified normal activity within six months, while those diagnosed late face permanent activity restrictions and dependence on assistive devices.
Who is at risk and when to suspect Charcot foot
Your risk of developing Charcot foot increases dramatically if you have peripheral neuropathy combined with any condition that weakens your bones or alters your immune response. Diabetes accounts for 80% of Charcot foot cases, but the actual trigger is loss of protective sensation in your feet, not the diabetes itself. When you can’t feel pain from micro-fractures and ligament damage, you continue walking on an injured foot that would normally force you to rest.
Primary risk factors that trigger Charcot foot
Neuropathy from diabetes creates the perfect storm for Charcot foot when combined with recent foot surgery, infection, or trauma. Your body launches an inflammatory response to these events, releasing chemicals that inadvertently soften bone and weaken the structural supports in your foot. You face elevated risk during the first year after any foot procedure, during active foot infections, or within months of uncontrolled blood sugar episodes that damage nerves further.
Other conditions that increase your vulnerability include chronic kidney disease, peripheral vascular disease, and any neurological disorder that reduces sensation in your feet. Patients taking immunosuppressive medications or those with rheumatoid arthritis show higher Charcot foot rates because inflammation plays a central role in bone destruction. Understanding how Charcot foot is diagnosed starts with recognizing these risk factors in your medical history.
If you have diabetes with neuropathy and your foot suddenly becomes warm, red, and swollen after minor trauma or surgery, you need evaluation within 24 to 48 hours.
Warning signs that should prompt immediate evaluation
Suspect Charcot foot when you notice unilateral warmth and swelling in your foot or ankle, especially if you can’t recall a specific injury that would explain the symptoms. Your affected foot feels 3 to 6 degrees warmer than your other foot when you touch both simultaneously. This temperature difference, combined with redness that doesn’t fade when you elevate your leg, signals active bone and joint destruction.
Recent changes in your daily routine matter. Starting a new exercise program, increasing your walking distance, or standing for longer periods than usual can trigger Charcot foot in patients with established neuropathy. Your foot swells progressively over days to weeks rather than appearing overnight, and the swelling doesn’t respond to typical measures like elevation or compression that would help a simple sprain.
Key symptoms and visible signs clinicians look for
Your doctor evaluates specific physical findings that distinguish Charcot foot from similar conditions during the diagnostic process. Understanding how Charcot foot is diagnosed begins with recognizing the classic symptom pattern that appears in the acute phase. Your foot shows warmth, redness, and swelling, yet you report minimal or no pain despite obvious inflammation. This painless presentation in a patient with known neuropathy immediately raises suspicion for active Charcot foot rather than infection or injury.
The hallmark presentation of acute Charcot foot
Clinicians look for unilateral warmth with temperature differences between your affected and unaffected foot ranging from 3 to 10 degrees Fahrenheit. Your doctor will touch both feet simultaneously to feel this difference, which you might not notice yourself due to neuropathy. The warmth concentrates over joints in your midfoot or ankle rather than spreading diffusely across your entire foot, pointing to active bone and joint inflammation rather than cellulitis.

Swelling appears disproportionate to any trauma you recall, often developing gradually over several days. Your foot looks puffy and feels tight, with skin that appears shiny and stretched. Unlike edema from heart or kidney problems that affects both feet equally, Charcot foot swelling stays confined to one foot and doesn’t pit easily when you press on it. Your affected foot may appear wider than your other foot, especially across the midfoot where joints are loosening.
The combination of a warm, swollen, painless foot in a patient with neuropathy should trigger immediate evaluation for Charcot foot, even without visible deformity.
Physical changes that develop as the condition progresses
Early structural changes include loss of your normal arch height when you stand, which your doctor measures by checking the distance between your arch and the floor. Your foot may feel unstable when you walk, as if the bones are shifting position with each step. Clinicians look for altered weight distribution patterns by examining where calluses form on your sole, since abnormal pressure points develop before visible deformity appears.
Advanced signs include visible collapse of your midfoot creating a convex bulge on your sole, though catching Charcot foot before this stage develops remains the goal. Your doctor checks for instability by gently moving joints in your foot, feeling for abnormal motion that indicates ligament failure and joint dislocation.
What to expect during the foot and ankle exam
Your doctor begins the physical examination by comparing both feet simultaneously, looking for differences in appearance, temperature, and structural alignment. This comparative approach reveals subtle asymmetries that you might not notice on your own. The exam takes place with you sitting on the examination table with both legs extended, allowing your clinician to observe foot positioning at rest before checking how your feet respond to movement and pressure. Understanding how Charcot foot is diagnosed through physical examination helps you prepare for what your doctor will assess during your appointment.
Temperature assessment and palpation techniques
Your clinician uses the back of their hand to feel both feet at the same time, checking for warmth differences across your ankles, midfoot, and forefoot. This direct comparison detects temperature variations as small as 2 to 3 degrees Fahrenheit, which indicate active inflammation in bone and joints. Your doctor presses gently along bone prominences and joint lines to identify areas of tenderness, though reduced sensation from neuropathy means you might not feel discomfort even when inflammation exists.
The palpation process includes checking your pulses at multiple points in your foot and ankle, since adequate blood flow affects both diagnosis and treatment planning. Your doctor feels for swelling consistency, noting whether fluid shifts when pressed or remains firm and non-pitting, which helps differentiate Charcot foot from other causes of swelling like heart failure or venous insufficiency.
A thorough temperature comparison between your feet provides one of the most reliable early indicators of active Charcot foot during physical examination.
Range of motion and stability testing
Your clinician moves each joint in your foot and ankle through its normal range, comparing mobility and endpoint feel between your affected and unaffected sides. Abnormal looseness or excessive motion in joints that should feel stable signals ligament damage and joint destruction characteristic of Charcot foot. Your doctor applies gentle stress to joints by moving your foot in specific directions while stabilizing your leg, checking whether bones shift position abnormally.
Weight-bearing assessment follows, with you standing while your doctor observes arch height, alignment, and how your foot contacts the floor. Your clinician watches how you walk, noting changes in your gait pattern or visible instability that suggest structural compromise even before deformity becomes obvious on X-rays.
Imaging used to diagnose Charcot foot
Your doctor orders specific imaging studies that reveal bone and joint changes invisible during physical examination, making imaging essential for confirming diagnosis and determining treatment. X-rays serve as the first-line imaging modality because they’re readily available, inexpensive, and show bone destruction and alignment changes that define each Charcot foot stage. Understanding how Charcot foot is diagnosed through imaging helps you recognize why your doctor may order multiple types of scans, since different imaging techniques reveal different aspects of the condition at various stages of progression.
X-ray findings in early and advanced stages
Standard weight-bearing X-rays taken from multiple angles show your foot’s bone alignment and structural integrity while you stand and bear weight normally. Your doctor looks for fractures, dislocations, and bone debris scattered through joints, though early-stage Charcot foot may show minimal changes on initial X-rays despite active disease. The first visible signs include subtle bone demineralization, hairline fractures in metatarsals or tarsal bones, and joint space widening where ligaments have loosened but bones haven’t yet shifted position.
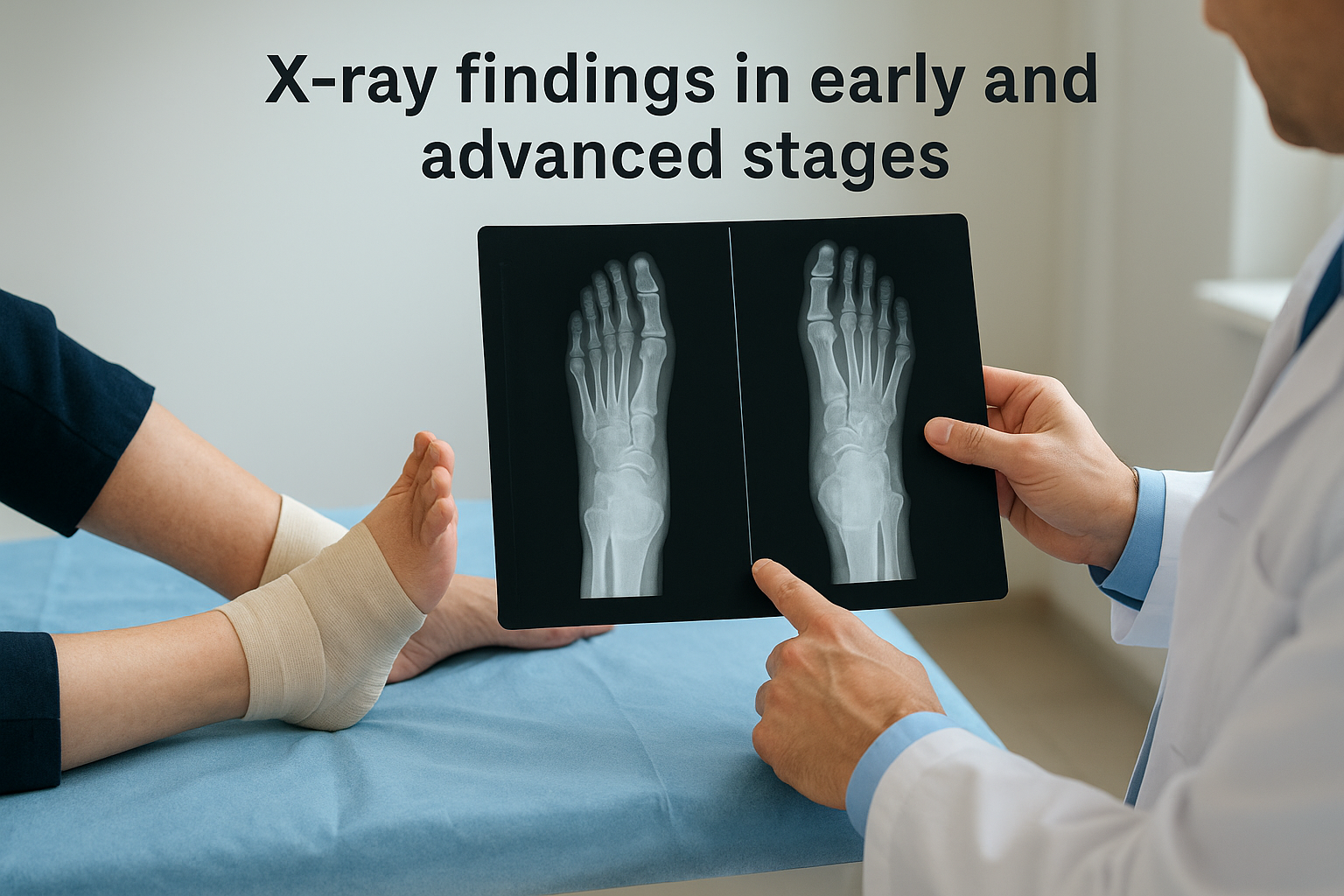
Progressive X-ray changes document your condition’s advancement through stages. Your images may reveal fragmentation of bone into multiple pieces, collapse of your arch structure, and displacement of joints from their normal positions. Comparison films taken weeks apart show whether bone destruction is advancing or stabilizing, information that guides your treatment intensity and determines when you can safely increase weight-bearing activity.
Serial X-rays over 4 to 6 weeks provide the most reliable method for tracking whether your Charcot foot is responding to immobilization or continuing to deteriorate.
MRI and specialized imaging when diagnosis is unclear
Your doctor orders an MRI scan when X-rays appear normal but your clinical presentation strongly suggests active Charcot foot, since MRI detects bone marrow edema and soft tissue inflammation weeks before X-ray changes appear. MRI imaging reveals early bone stress patterns and ligament damage that X-rays miss, allowing diagnosis at stage 0 when intervention prevents structural collapse. This advanced imaging distinguishes between infection and Charcot foot by showing characteristic patterns of bone and soft tissue involvement.
Nuclear medicine bone scans detect increased metabolic activity in your bones and joints, though they lack the specificity to differentiate Charcot foot from infection or other inflammatory conditions. Your doctor may order specialized imaging like CT scans for surgical planning, which provide detailed three-dimensional views of bone fragment positions and help surgeons determine optimal hardware placement if reconstruction becomes necessary.
How doctors rule out infection, gout, and DVT
Your doctor must systematically exclude conditions that produce similar symptoms before confirming Charcot foot, since misdiagnosis leads to inappropriate treatment that worsens outcomes. Cellulitis, osteomyelitis, gout, and deep vein thrombosis all cause warmth, redness, and swelling that mimic Charcot foot’s presentation. Understanding how Charcot foot is diagnosed includes recognizing the specific tests and clinical findings that separate these conditions, since treating infection with immobilization or treating Charcot foot with antibiotics both create serious complications.
Laboratory tests and imaging patterns that distinguish infection
Your clinician orders blood tests measuring inflammatory markers including white blood cell count, erythrocyte sedimentation rate, and C-reactive protein to assess for active infection. Elevated white blood cell counts with left shift suggest bacterial infection, while normal or mildly elevated inflammatory markers support Charcot foot diagnosis. Your doctor collects blood cultures if you have fever or systemic symptoms, since bacteremia indicates spreading infection requiring immediate antibiotic treatment rather than casting.
MRI imaging reveals distinct patterns between infection and Charcot foot that guide diagnosis. Osteomyelitis shows focal bone destruction with adjacent soft tissue abscess formation and sinus tracts, while Charcot foot produces diffuse bone marrow edema across multiple bones without soft tissue fluid collections. Your doctor looks for skin breaks or ulcers that provide entry points for bacteria, since infection rarely develops in intact skin while Charcot foot occurs without open wounds in early stages.
Laboratory markers combined with MRI patterns provide definitive differentiation between infection and Charcot foot when clinical presentation remains ambiguous.
Clinical features that separate gout and DVT from Charcot foot
Gout typically affects your big toe joint with sudden, severe pain that patients with neuropathy can still feel due to inflammation’s intensity, while Charcot foot produces minimal discomfort despite dramatic swelling. Your doctor may aspirate joint fluid to check for uric acid crystals under microscopy, which confirms gout and excludes Charcot foot. Gout responds rapidly to anti-inflammatory medications within 24 to 48 hours, whereas Charcot foot swelling persists despite these treatments.
Deep vein thrombosis causes leg swelling extending above your ankle into your calf, while Charcot foot swelling stays confined to your foot and ankle. Your clinician orders duplex ultrasound to visualize blood flow and detect clots when DVT remains a possibility, since both conditions require different management approaches.
What happens after diagnosis and next steps
Your treatment begins immediately after your doctor confirms Charcot foot diagnosis, with complete non-weight-bearing or protected weight-bearing as the cornerstone of early intervention. Your clinician fits you with a total contact cast or removable boot within 24 to 48 hours of diagnosis to prevent further bone destruction and joint collapse. The first weeks after understanding how Charcot foot is diagnosed determine whether you’ll preserve your foot’s structure or face progressive deformity, making strict adherence to offloading protocols your most critical responsibility during acute treatment.
Immediate immobilization and offloading protocol
Your doctor applies a total contact cast extending from your toes to below your knee, distributing pressure evenly across your entire foot and lower leg to eliminate stress on damaged bones and joints. You’ll use crutches, a knee scooter, or wheelchair for mobility since complete non-weight-bearing for the first 4 to 8 weeks prevents further fracture displacement. Your cast requires replacement every 1 to 2 weeks initially as swelling decreases, with each cast change including X-rays to monitor bone healing and verify that destruction hasn’t progressed.
Removable controlled ankle motion boots serve as an alternative when you can’t tolerate casting or need access for wound care, though compliance becomes critical since removing the boot to walk undermines treatment effectiveness. Your clinician prescribes specific weight-bearing restrictions ranging from total non-weight-bearing to touch-down weight-bearing, with progression based on X-ray findings and temperature normalization rather than time elapsed.
Your foot temperature must decrease to within 2 degrees Fahrenheit of your unaffected foot before your doctor allows increased weight-bearing, typically requiring 8 to 12 weeks of strict immobilization.
Monitoring schedule and treatment progression
Follow-up appointments occur every 2 to 4 weeks during acute treatment, with each visit including temperature measurements, X-rays, and clinical examination to track your response to immobilization. Your doctor looks for decreased warmth, reduced swelling, and stable bone positions on serial X-rays as signs of successful healing. Treatment extends 12 to 18 weeks on average, though some patients require 6 to 9 months of protected weight-bearing before achieving complete temperature normalization and bone consolidation.
Transition to custom orthotic devices and specialized footwear follows successful acute treatment, with your doctor gradually increasing your activity level while monitoring for any temperature elevation that signals recurrent inflammation.
Next steps
Understanding how Charcot foot is diagnosed empowers you to recognize warning signs before permanent damage occurs. Your immediate action matters most when you notice unexplained warmth, redness, or swelling in your foot, especially if you have diabetes or neuropathy. Don’t wait for pain to develop, since neuropathy masks the discomfort that would normally signal serious problems.
Schedule an evaluation within 24 to 48 hours if you suspect Charcot foot based on the symptoms described in this guide. Early intervention preserves your foot structure and avoids the complex surgeries required for advanced stages. Your doctor will perform the physical examination, order appropriate imaging, and start treatment immediately if Charcot foot is confirmed.
At Achilles Foot and Ankle Center, our specialists diagnose and treat Charcot foot across our Central Virginia locations using advanced imaging technology and specialized expertise in diabetic foot care. Make a same-day appointment to get the evaluation you need when timing matters most.